Tiroides De Hashimoto, also known as Hashimoto's Thyroiditis, is a prevalent autoimmune disorder where the immune system mistakenly attacks the thyroid gland. This condition, named after the Japanese physician who first described it, Dr. Hakaru Hashimoto, can lead to hypothyroidism, a condition characterized by an underactive thyroid. Tiroides De Hashimoto is one of the most common causes of hypothyroidism in the world, affecting millions of people, predominantly women. Understanding the nuances of this disorder is crucial for effective management and treatment, ensuring that individuals lead healthy and balanced lives.
In recent years, awareness about autoimmune disorders, including Tiroides De Hashimoto, has grown significantly, highlighting the importance of early diagnosis and intervention. The thyroid gland, a small butterfly-shaped organ located at the base of the neck, plays a critical role in regulating metabolism, energy levels, and overall body temperature. When the thyroid is compromised due to autoimmune attacks, as in the case of Tiroides De Hashimoto, it can lead to a host of symptoms such as fatigue, weight gain, depression, and more. Despite its prevalence, many remain unaware of the symptoms and potential complications of this condition, emphasizing the need for comprehensive information and guidance.
Thankfully, advancements in medical research and treatment have made it possible to manage Tiroides De Hashimoto effectively. This article aims to provide an in-depth exploration of this condition, offering insights into its causes, symptoms, diagnosis, and treatment options. By understanding the science behind Tiroides De Hashimoto and adopting appropriate lifestyle changes, individuals can mitigate its impact and enhance their quality of life. Whether you are newly diagnosed, have been managing the condition for years, or are simply seeking to educate yourself, this guide serves as a valuable resource for navigating the complexities of Tiroides De Hashimoto.
Table of Contents
- What is Tiroides De Hashimoto?
- Causes of Tiroides De Hashimoto
- Symptoms of Tiroides De Hashimoto
- Diagnosis of Tiroides De Hashimoto
- Treatment Options for Tiroides De Hashimoto
- Lifestyle Changes and Management
- Dietary Considerations
- Exercise and Physical Activity
- Potential Complications
- Living with Tiroides De Hashimoto
- Support and Resources
- Frequently Asked Questions
- Conclusion
What is Tiroides De Hashimoto?
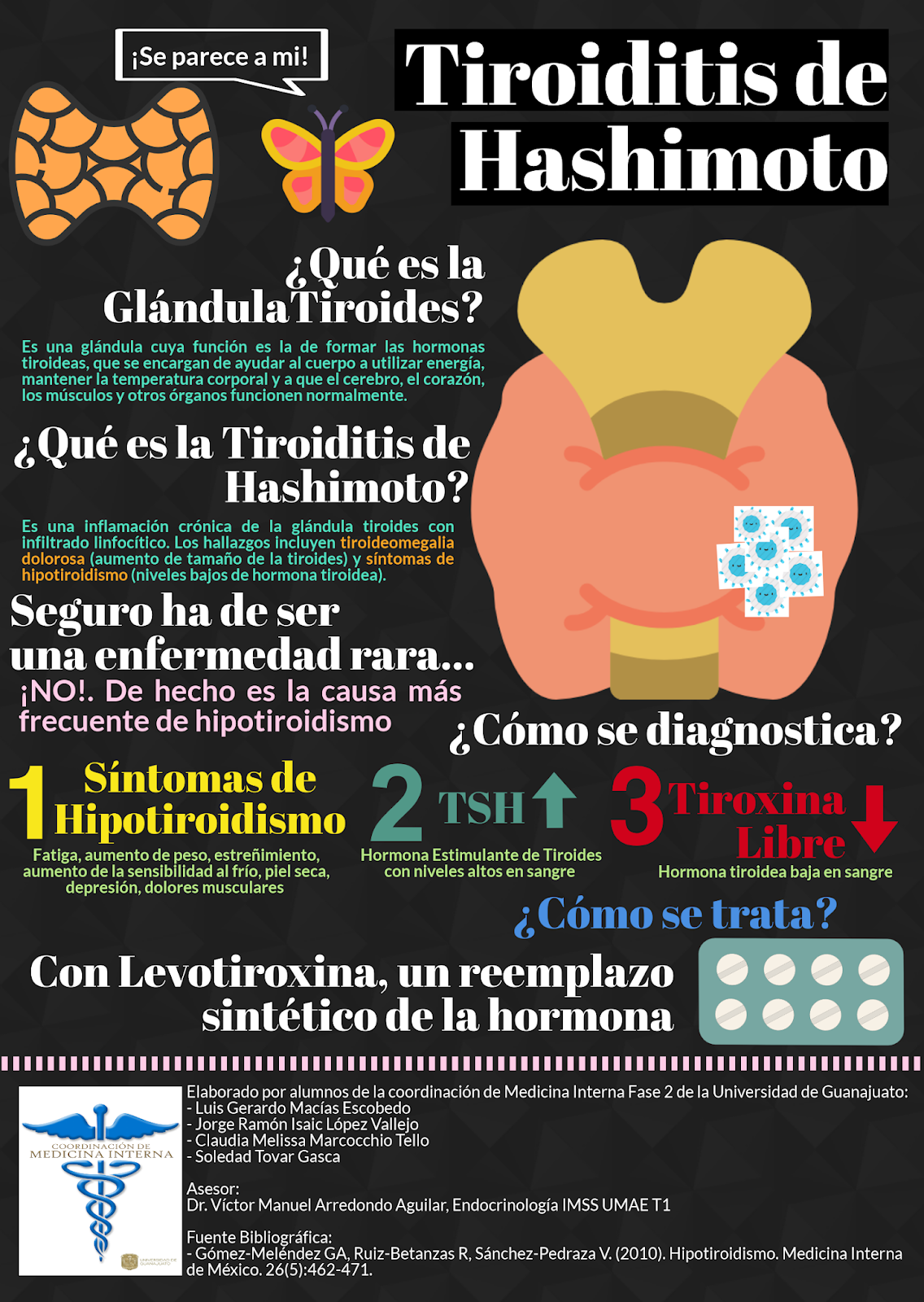
Tiroides De Hashimoto is an autoimmune disorder that affects the thyroid gland, leading to chronic inflammation and often resulting in an underactive thyroid, or hypothyroidism. The thyroid gland is part of the endocrine system, responsible for producing hormones that regulate metabolism, energy, and other vital functions. In Tiroides De Hashimoto, the body's immune system mistakenly identifies the thyroid as a threat and begins to attack it, impairing its ability to function properly.
This condition was first described in 1912 by Dr. Hakaru Hashimoto, who identified the characteristic lymphocytic infiltration of the thyroid gland. It is the most common cause of hypothyroidism in iodine-sufficient areas and can affect individuals of any age, though it is most frequently diagnosed in middle-aged women. The exact cause of Tiroides De Hashimoto remains unknown, but it is believed to result from a combination of genetic, environmental, and hormonal factors.
While Tiroides De Hashimoto can be asymptomatic in its early stages, it often progresses to cause symptoms associated with reduced thyroid hormone levels. These can include fatigue, cold intolerance, weight gain, depression, and muscle weakness, among others. Understanding the nature of Tiroides De Hashimoto is essential for timely diagnosis and effective management, preventing further complications and improving the patient's quality of life.
Causes of Tiroides De Hashimoto
The exact cause of Tiroides De Hashimoto is not fully understood, but it is believed to be the result of a combination of genetic and environmental factors. Research suggests that there is a hereditary component to the disorder, as it tends to run in families. Individuals with a family history of autoimmune diseases are at a higher risk of developing Tiroides De Hashimoto.
Environmental factors also play a significant role in the development of the condition. These can include exposure to certain viruses or bacteria, which may trigger the immune system to attack the thyroid gland. Additionally, high levels of stress, dietary deficiencies, and excessive iodine intake have been linked to an increased risk of autoimmune thyroiditis.
Hormonal imbalances, particularly in women, are another contributing factor. Women are significantly more likely than men to develop Tiroides De Hashimoto, suggesting that hormonal changes during puberty, pregnancy, and menopause may influence the onset of the disorder. Understanding these causes can help in identifying individuals at risk and implementing preventive measures to mitigate the impact of the disease.
Symptoms of Tiroides De Hashimoto
Symptoms of Tiroides De Hashimoto can vary widely among individuals and often develop gradually over time. In the initial stages, many people may not experience any noticeable symptoms, leading to delayed diagnosis and treatment. However, as the condition progresses and thyroid hormone levels decrease, various symptoms may manifest.
Common symptoms of Tiroides De Hashimoto include chronic fatigue, unexplained weight gain, sensitivity to cold, dry skin, hair loss, and muscle weakness. Individuals may also experience constipation, depression, memory problems, and a slowed heart rate. Women may notice changes in their menstrual cycles, including heavy or irregular periods.
In some cases, the thyroid gland may become enlarged, a condition known as a goiter, which can lead to a visible swelling at the base of the neck. It is important to note that the severity of symptoms does not always correlate with the degree of thyroid dysfunction, making it essential for individuals to seek medical evaluation if they suspect a thyroid issue.
Diagnosis of Tiroides De Hashimoto
Diagnosing Tiroides De Hashimoto typically involves a combination of clinical evaluation, laboratory tests, and imaging studies. A healthcare provider will begin by taking a detailed medical history and conducting a physical examination, focusing on symptoms and any noticeable changes in the thyroid gland.
Blood tests are crucial in diagnosing Tiroides De Hashimoto, as they can measure levels of thyroid hormones (T3 and T4) and thyroid-stimulating hormone (TSH). In individuals with Hashimoto's Thyroiditis, TSH levels are often elevated due to the pituitary gland's attempt to stimulate the underactive thyroid. Additionally, tests for specific antibodies, such as anti-thyroid peroxidase (TPO) antibodies and anti-thyroglobulin antibodies, can confirm the autoimmune nature of the condition.
In some cases, an ultrasound of the thyroid may be performed to assess the gland's size and structure, identifying any nodules or irregularities. Early detection through these diagnostic methods is essential for initiating appropriate treatment and preventing further complications associated with Tiroides De Hashimoto.
Treatment Options for Tiroides De Hashimoto
Treatment for Tiroides De Hashimoto aims to restore normal thyroid function and alleviate symptoms. The primary approach involves hormone replacement therapy, using synthetic thyroid hormone levothyroxine to normalize thyroid hormone levels. Levothyroxine is typically taken orally once a day and is adjusted based on regular monitoring of thyroid function tests.
While levothyroxine effectively manages symptoms for most individuals, some may require additional medications or adjustments to achieve optimal thyroid function. It is essential for patients to work closely with their healthcare provider to determine the appropriate dosage and treatment plan, considering factors such as age, weight, and the presence of other medical conditions.
In addition to medication, addressing lifestyle factors and dietary considerations can support overall well-being and improve the management of Tiroides De Hashimoto. Patients are encouraged to maintain regular follow-up appointments and communicate any changes in symptoms to their healthcare provider promptly.
Lifestyle Changes and Management
Adopting a healthy lifestyle is crucial for managing Tiroides De Hashimoto effectively. Patients are encouraged to focus on balanced nutrition, regular physical activity, stress reduction, and adequate sleep. These factors can enhance overall health and mitigate the impact of thyroid dysfunction.
Maintaining a balanced diet rich in essential nutrients, such as iodine, selenium, and zinc, can support thyroid function. However, it is important to avoid excessive iodine intake, which can exacerbate thyroid issues. Consulting with a registered dietitian or nutritionist can help tailor a diet plan that meets individual needs and supports thyroid health.
Regular physical activity, such as walking, swimming, or yoga, can improve energy levels, mood, and metabolism. It is important for individuals with Tiroides De Hashimoto to find activities they enjoy and can sustain over time. Additionally, stress management techniques, such as meditation, deep breathing exercises, and mindfulness, can help reduce the impact of stress on the immune system and thyroid function.
Dietary Considerations
Diet plays a significant role in managing Tiroides De Hashimoto, as certain nutrients and food components can influence thyroid health. Patients are encouraged to consume a nutrient-rich diet that includes a variety of fruits, vegetables, lean proteins, and whole grains. Key nutrients for thyroid health include iodine, selenium, zinc, and vitamin D.
Iodine is essential for thyroid hormone production, but excessive intake can exacerbate autoimmune thyroiditis. It is important for individuals with Tiroides De Hashimoto to monitor their iodine intake and avoid high-iodine foods, such as seaweed and iodized salt. Selenium and zinc are important for supporting the immune system and thyroid function and can be found in foods such as Brazil nuts, fish, poultry, and legumes.
Vitamin D deficiency has been linked to autoimmune disorders, including Tiroides De Hashimoto. Ensuring adequate vitamin D levels through sunlight exposure, diet, or supplements can support immune health and thyroid function. Patients are encouraged to work with their healthcare provider or dietitian to develop a personalized nutrition plan that supports their specific needs and goals.
Exercise and Physical Activity
Regular physical activity is an important component of managing Tiroides De Hashimoto, as it can help improve energy levels, mood, and overall health. Exercise can also support weight management, which is often a concern for individuals with hypothyroidism. Patients are encouraged to incorporate a mix of cardiovascular, strength, and flexibility exercises into their routine.
Cardiovascular exercises, such as walking, cycling, or swimming, can boost energy levels and promote cardiovascular health. Strength training exercises, such as weightlifting or resistance band workouts, can help maintain muscle mass and support metabolism. Additionally, flexibility exercises, such as yoga or stretching, can improve joint mobility and reduce the risk of injury.
It is important for individuals with Tiroides De Hashimoto to find activities they enjoy and can sustain over time, as consistency is key to reaping the benefits of exercise. Patients are encouraged to consult with their healthcare provider or a fitness professional to develop a personalized exercise plan that meets their needs and goals.
Potential Complications
While Tiroides De Hashimoto is a manageable condition, untreated or poorly managed cases can lead to a range of complications. One of the most common complications is goiter, an enlargement of the thyroid gland that can cause discomfort and difficulty swallowing or breathing. In some cases, goiter may require surgical intervention.
Another potential complication is heart problems, as hypothyroidism can lead to elevated cholesterol levels and an increased risk of heart disease. Proper management of thyroid hormone levels and lifestyle modifications can help mitigate these risks. Additionally, untreated Tiroides De Hashimoto can lead to mental health issues, such as depression and anxiety, due to the impact of thyroid hormones on brain function and mood regulation.
In severe cases, untreated hypothyroidism can lead to myxedema coma, a rare but life-threatening condition characterized by extreme fatigue, hypothermia, and altered mental status. Early diagnosis and treatment are crucial to prevent these complications and maintain overall health and well-being.
Living with Tiroides De Hashimoto
Living with Tiroides De Hashimoto requires a proactive approach to health management, focusing on medication adherence, lifestyle modifications, and regular monitoring. Patients are encouraged to take their prescribed medications as directed and communicate with their healthcare provider about any changes in symptoms or concerns.
In addition to medical management, individuals with Tiroides De Hashimoto can benefit from building a support network of family, friends, and healthcare professionals. Support groups and online communities can provide valuable resources, information, and encouragement for those living with the condition.
Patients are also encouraged to educate themselves about Tiroides De Hashimoto and stay informed about new research and treatment options. By taking an active role in their health management, individuals can enhance their quality of life and reduce the impact of the condition on their daily activities.
Support and Resources
Access to support and resources is essential for individuals living with Tiroides De Hashimoto. Healthcare providers, including endocrinologists, primary care physicians, and dietitians, play a crucial role in managing the condition and providing guidance on treatment and lifestyle modifications.
Support groups and online communities can offer valuable information, encouragement, and a sense of community for those living with Tiroides De Hashimoto. Organizations such as the American Thyroid Association and the Thyroid Foundation of Canada provide educational materials, resources, and support for patients and their families.
Patients are encouraged to utilize these resources and seek support from their healthcare providers, family, and friends to navigate the challenges of living with Tiroides De Hashimoto and achieve optimal health and well-being.
Frequently Asked Questions
1. What is the main cause of Tiroides De Hashimoto?
Tiroides De Hashimoto is primarily caused by a combination of genetic, environmental, and hormonal factors. It is an autoimmune disorder where the immune system mistakenly attacks the thyroid gland, leading to inflammation and reduced thyroid function.
2. Can Tiroides De Hashimoto be cured?
There is currently no cure for Tiroides De Hashimoto, but the condition can be effectively managed with medication and lifestyle modifications. Hormone replacement therapy with levothyroxine is the standard treatment to restore normal thyroid function.
3. What dietary changes should I make if I have Tiroides De Hashimoto?
Individuals with Tiroides De Hashimoto are encouraged to consume a balanced diet rich in essential nutrients, such as iodine, selenium, zinc, and vitamin D. It is important to avoid excessive iodine intake and focus on whole, nutrient-dense foods to support thyroid health.
4. How does exercise help manage Tiroides De Hashimoto?
Regular exercise can improve energy levels, mood, and metabolism, which are often affected by hypothyroidism. A combination of cardiovascular, strength, and flexibility exercises can support overall health and well-being for individuals with Tiroides De Hashimoto.
5. What are the potential complications of untreated Tiroides De Hashimoto?
Untreated Tiroides De Hashimoto can lead to complications such as goiter, heart problems, mental health issues, and, in severe cases, myxedema coma. Early diagnosis and treatment are essential to prevent these complications and maintain overall health.
6. Can stress affect Tiroides De Hashimoto?
Yes, stress can exacerbate autoimmune conditions like Tiroides De Hashimoto. Stress management techniques, such as meditation, yoga, and mindfulness, can help reduce the impact of stress on the immune system and thyroid function.
Conclusion
In conclusion, Tiroides De Hashimoto is a common autoimmune disorder that affects the thyroid gland and can lead to hypothyroidism. Understanding the causes, symptoms, diagnosis, and treatment options is crucial for effective management and improved quality of life. By adopting a proactive approach to health management, including medication adherence, lifestyle modifications, and regular monitoring, individuals with Tiroides De Hashimoto can mitigate the impact of the condition and lead fulfilling lives.
Access to support and resources is essential for navigating the challenges of living with Tiroides De Hashimoto. Patients are encouraged to seek guidance from healthcare providers, utilize support groups and online communities, and stay informed about new research and treatment options. With the right support and management strategies, individuals with Tiroides De Hashimoto can achieve optimal health and well-being.
For more information on Tiroides De Hashimoto and thyroid health, consider visiting the American Thyroid Association website for valuable resources and educational materials.
Article Recommendations