Tiroides Hashimoto, also known as Hashimoto's thyroiditis, is an autoimmune disorder that affects the thyroid gland, a small organ located at the base of the neck. This condition occurs when the immune system mistakenly attacks the thyroid gland, leading to inflammation and often resulting in hypothyroidism, a condition where the thyroid fails to produce enough hormones. Affecting millions of people worldwide, Tiroides Hashimoto is a leading cause of hypothyroidism, especially among women. Understanding the intricacies of this disorder is crucial for effective management and treatment.
The growing prevalence of Tiroides Hashimoto and its impact on individuals' lives necessitates a comprehensive exploration of its causes, symptoms, diagnosis, and treatment options. While the exact cause of Tiroides Hashimoto remains unknown, several factors such as genetics, environmental triggers, and hormonal changes have been identified as potential contributors. The disorder manifests through a range of symptoms, including fatigue, weight gain, depression, and sensitivity to cold, which can significantly affect the quality of life if left unmanaged.
Through this detailed article, we aim to provide a thorough understanding of Tiroides Hashimoto, offering insights into its pathophysiology, risk factors, and the latest advancements in its diagnosis and treatment. By delving into the complexities of this autoimmune disorder, we hope to equip readers with the knowledge necessary to recognize its symptoms, seek appropriate medical care, and explore strategies for effectively managing the condition. Whether you are newly diagnosed, a healthcare professional, or someone seeking to support a loved one, this article serves as a comprehensive guide to navigating the challenges posed by Tiroides Hashimoto.
Table of Contents
- What is Tiroides Hashimoto?
- Causes of Tiroides Hashimoto
- Symptoms and Signs
- Diagnosis
- Treatment Options
- Lifestyle and Dietary Considerations
- Impact on Daily Life
- Living with Tiroides Hashimoto
- Psychological Aspects
- Impact on Reproductive Health
- Risk Factors
- Current Research and Future Directions
- Support and Resources
- Frequently Asked Questions
- Conclusion
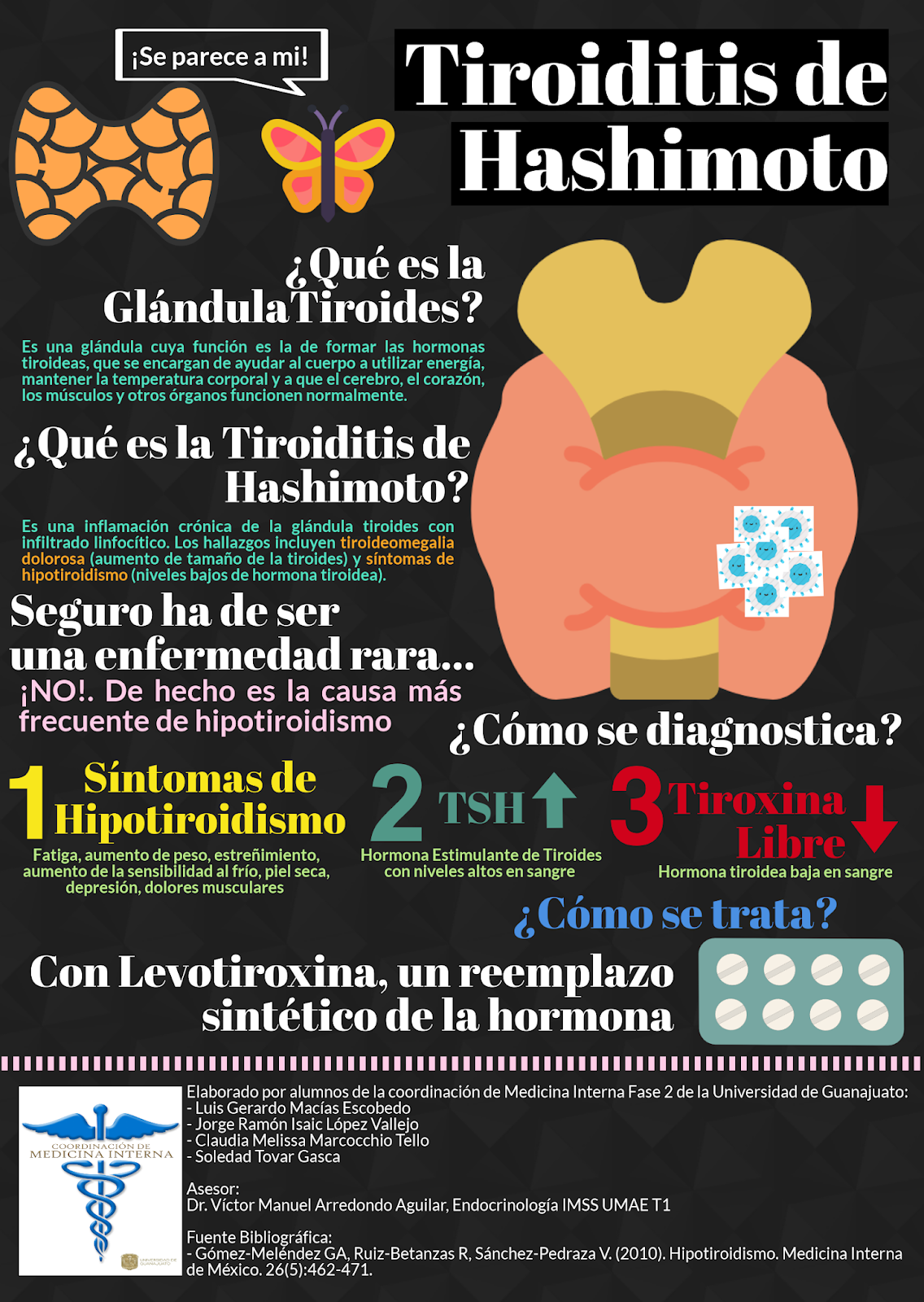
What is Tiroides Hashimoto?
Tiroides Hashimoto, or Hashimoto's thyroiditis, is a chronic autoimmune disease where the body's immune system attacks the thyroid gland. This gland is responsible for producing hormones that regulate the body's metabolism, energy levels, and many other critical functions. The autoimmune attack leads to chronic inflammation and often results in an underactive thyroid, known as hypothyroidism.
Hashimoto's was first described in 1912 by the Japanese physician Hakaru Hashimoto. It is the most common cause of hypothyroidism in areas where iodine levels are sufficient. The disorder is more prevalent in women, occurring at a ratio of approximately 7:1 compared to men. It typically manifests in middle age but can affect individuals of any age, including children and the elderly.
The disease's progression is often slow, with symptoms gradually worsening over time. Early detection and management are crucial to avoid complications such as heart disease, mental health issues, and infertility. Understanding Tiroides Hashimoto involves recognizing its symptoms, undergoing proper testing, and adhering to a treatment plan tailored to individual needs.
Causes of Tiroides Hashimoto
The exact cause of Tiroides Hashimoto remains unknown, but it is believed to result from a combination of genetic, environmental, and hormonal factors. Understanding these causes can help in the early identification and management of the condition.
Genetic Factors
Genetic predisposition plays a significant role in the development of Tiroides Hashimoto. Studies have shown that individuals with a family history of thyroid disorders or other autoimmune diseases are at a higher risk of developing Hashimoto's thyroiditis. Several genes have been associated with an increased susceptibility to the disorder, although the exact genetic mechanisms remain under investigation.
Environmental Triggers
Environmental factors such as exposure to radiation, excessive iodine intake, and viral infections may trigger the onset of Tiroides Hashimoto in genetically predisposed individuals. In areas with high iodine consumption, a higher incidence of autoimmune thyroid diseases, including Hashimoto's, has been observed. Additionally, certain infections may disrupt the immune system, potentially initiating an autoimmune response against the thyroid gland.
Hormonal Changes
Hormonal fluctuations, particularly in women, have been linked to Tiroides Hashimoto. The disorder is more prevalent in women, especially during periods of hormonal change such as puberty, pregnancy, and menopause. This suggests that hormonal factors may influence the immune system's response to the thyroid gland.
Symptoms and Signs
Tiroides Hashimoto can present with a wide range of symptoms, many of which overlap with other conditions, making diagnosis challenging. Symptoms can vary in severity and may develop gradually over several years.
Common Symptoms
Common symptoms of Tiroides Hashimoto include fatigue, weight gain, and cold intolerance. Patients may also experience dry skin, hair loss, constipation, and muscle weakness. These symptoms result from the reduced production of thyroid hormones, which slows down the body's metabolic processes.
Mental Health Symptoms
Hashimoto's can also impact mental health, leading to symptoms such as depression, anxiety, and cognitive difficulties. These psychological symptoms can significantly affect an individual's quality of life and often improve with appropriate thyroid hormone replacement therapy.
Physical Examination Findings
During a physical examination, a healthcare provider may detect an enlarged thyroid gland, known as a goiter, in individuals with Tiroides Hashimoto. The presence of a goiter may indicate chronic thyroid inflammation and should be further evaluated through blood tests and imaging studies.
Diagnosis
Diagnosing Tiroides Hashimoto involves a combination of clinical evaluation, blood tests, and imaging studies. Early diagnosis is essential for effective management and prevention of complications.
Clinical Evaluation
The diagnostic process begins with a thorough clinical evaluation, where a healthcare provider reviews the patient's medical history and performs a physical examination. The presence of symptoms such as fatigue, weight gain, and goiter may raise suspicion of Hashimoto's thyroiditis.
Blood Tests
Blood tests are crucial in confirming the diagnosis of Tiroides Hashimoto. These tests typically include measuring levels of thyroid-stimulating hormone (TSH), free thyroxine (T4), and thyroid peroxidase antibodies (TPOAb). Elevated TSH and low T4 levels indicate hypothyroidism, while the presence of TPOAb suggests an autoimmune process targeting the thyroid gland.
Imaging Studies
In some cases, imaging studies such as ultrasound may be performed to assess the size and structure of the thyroid gland. Ultrasound can help identify nodules or other structural abnormalities that may require further evaluation.
Treatment Options
The primary goal of treating Tiroides Hashimoto is to restore normal thyroid hormone levels and alleviate symptoms. Treatment is individualized based on the severity of the condition and the patient's overall health.
Thyroid Hormone Replacement Therapy
Thyroid hormone replacement therapy is the cornerstone of treatment for Tiroides Hashimoto. Levothyroxine, a synthetic form of the thyroid hormone thyroxine (T4), is commonly prescribed to normalize hormone levels and relieve symptoms. Treatment is typically lifelong, with regular monitoring to adjust the dosage as needed.
Monitoring and Follow-up
Regular follow-up with a healthcare provider is essential to monitor thyroid hormone levels and assess the effectiveness of treatment. Blood tests are usually performed every six to twelve months to ensure that hormone levels remain within the target range.
Addressing Associated Symptoms
In addition to hormone replacement therapy, treatment may also involve addressing associated symptoms such as depression or anxiety. This may include counseling, lifestyle modifications, and, in some cases, medication.
Lifestyle and Dietary Considerations
While medication is the primary treatment for Tiroides Hashimoto, lifestyle and dietary modifications can support overall health and well-being. Patients are encouraged to adopt a healthy lifestyle to complement medical treatment.
Dietary Recommendations
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support thyroid function and overall health. Some patients may benefit from reducing their intake of goitrogenic foods, such as cruciferous vegetables, which can interfere with thyroid hormone production when consumed in large amounts.
Exercise and Physical Activity
Regular physical activity is important for maintaining a healthy weight, improving energy levels, and boosting mood. Patients with Tiroides Hashimoto are encouraged to engage in moderate exercise, such as walking, swimming, or yoga, as part of their daily routine.
Stress Management
Stress management techniques, such as meditation, deep breathing exercises, and mindfulness, can help reduce stress levels and improve overall well-being. Chronic stress can negatively impact the immune system and thyroid function, making stress reduction an important aspect of managing Tiroides Hashimoto.
Impact on Daily Life
Living with Tiroides Hashimoto can present several challenges, affecting various aspects of daily life. Understanding these challenges and finding effective coping strategies are essential for maintaining a good quality of life.
Managing Fatigue
Fatigue is a common and often debilitating symptom of Tiroides Hashimoto. Patients can manage fatigue by prioritizing rest, establishing a consistent sleep schedule, and balancing activities to avoid overexertion.
Weight Management
Weight gain is a common concern for individuals with Tiroides Hashimoto. Adopting a healthy diet and engaging in regular physical activity can help manage weight and promote overall health. Patients may also benefit from working with a nutritionist or dietitian to develop a personalized plan.
Emotional Well-being
Living with a chronic condition like Tiroides Hashimoto can take an emotional toll. Seeking support from friends, family, or mental health professionals can help patients cope with the psychological impact of the disorder. Joining support groups or online communities can also provide a sense of connection and understanding.
Living with Tiroides Hashimoto
Successfully managing Tiroides Hashimoto requires a proactive approach to healthcare and lifestyle choices. Patients can take several steps to live well with the condition and minimize its impact on their daily lives.
Educating Yourself
Understanding Tiroides Hashimoto and its effects on the body is crucial for effective self-management. Patients are encouraged to educate themselves about the disorder, treatment options, and lifestyle modifications that can support their health.
Building a Healthcare Team
Establishing a strong healthcare team, including a primary care physician, endocrinologist, and other specialists as needed, is essential for comprehensive care. Regular communication with healthcare providers ensures that patients receive appropriate treatment and support.
Setting Realistic Goals
Setting realistic goals for managing symptoms and improving overall health can help patients stay motivated and focused. This may include goals related to diet, exercise, stress management, and medication adherence.
Psychological Aspects
The psychological impact of Tiroides Hashimoto should not be underestimated. The disorder can affect mental health and emotional well-being, leading to symptoms such as depression, anxiety, and cognitive difficulties.
Recognizing Mental Health Symptoms
Patients should be aware of the potential mental health symptoms associated with Tiroides Hashimoto and seek help if needed. Symptoms may include persistent sadness, anxiety, difficulty concentrating, and changes in sleep patterns.
Seeking Support
Support from mental health professionals, such as therapists or counselors, can be beneficial for managing the psychological aspects of Tiroides Hashimoto. Therapy can provide coping strategies, emotional support, and a safe space to discuss concerns.
Peer Support and Community
Connecting with others who have Tiroides Hashimoto can provide valuable support and encouragement. Peer support groups, both in-person and online, offer a sense of community and shared understanding, which can be comforting for individuals navigating similar challenges.
Impact on Reproductive Health
Tiroides Hashimoto can have implications for reproductive health, particularly in women. Understanding these implications and seeking appropriate medical care are important for individuals planning to conceive or experiencing fertility issues.
Fertility and Pregnancy
Hypothyroidism resulting from Tiroides Hashimoto can affect fertility and pregnancy outcomes. Proper management of thyroid hormone levels is crucial for optimizing fertility and ensuring a healthy pregnancy. Women with Hashimoto's thyroiditis should work closely with their healthcare providers to monitor thyroid function before and during pregnancy.
Menstrual Irregularities
Tiroides Hashimoto can cause menstrual irregularities, such as heavy or irregular periods, due to hormonal imbalances. Addressing thyroid hormone levels through treatment can help regulate menstrual cycles and alleviate related symptoms.
Postpartum Thyroiditis
Some women with Tiroides Hashimoto may experience postpartum thyroiditis, a temporary inflammation of the thyroid gland after childbirth. This condition can cause fluctuating thyroid hormone levels and requires careful monitoring and management.
Risk Factors
Several risk factors have been identified for Tiroides Hashimoto, increasing the likelihood of developing the disorder. Understanding these risk factors can aid in early detection and intervention.
Genetic Predisposition
A family history of thyroid disorders or other autoimmune diseases is a significant risk factor for Tiroides Hashimoto. Individuals with relatives affected by these conditions should be vigilant for symptoms and seek medical evaluation if needed.
Gender and Age
Women are more likely to develop Tiroides Hashimoto than men, particularly during middle age. Hormonal changes during puberty, pregnancy, and menopause may contribute to this increased risk.
Environmental and Lifestyle Factors
Environmental factors, such as exposure to radiation or excessive iodine intake, may increase the risk of developing Tiroides Hashimoto. Lifestyle factors, including stress and smoking, can also impact immune function and thyroid health.
Current Research and Future Directions
Ongoing research into Tiroides Hashimoto aims to improve understanding of its causes, diagnosis, and treatment. Advances in scientific knowledge may lead to more effective therapies and management strategies in the future.
Genetic Research
Genetic research is focused on identifying the specific genes and genetic pathways involved in Tiroides Hashimoto. Understanding the genetic basis of the disorder may lead to targeted therapies and personalized treatment approaches.
Immunological Studies
Immunological studies aim to elucidate the mechanisms underlying the autoimmune response in Tiroides Hashimoto. Insights from these studies may inform the development of novel immunomodulatory treatments to prevent or mitigate the immune attack on the thyroid gland.
Innovations in Treatment
Research into new treatment options, including biologic therapies and advanced hormone replacement formulations, is ongoing. These innovations have the potential to improve symptom control and quality of life for individuals with Tiroides Hashimoto.
Support and Resources
Access to support and resources is essential for individuals living with Tiroides Hashimoto. Various organizations and online platforms provide information, guidance, and a sense of community for patients and their families.
Patient Advocacy Organizations
Organizations such as the American Thyroid Association and the British Thyroid Foundation offer resources and support for individuals affected by Tiroides Hashimoto. These organizations provide educational materials, research updates, and advocacy for thyroid health.
Online Communities
Online communities and social media platforms offer a space for individuals with Tiroides Hashimoto to connect, share experiences, and offer support. Engaging with these communities can provide valuable insights and encouragement for managing the disorder.
Healthcare Provider Support
Regular check-ins with healthcare providers are essential for ongoing management of Tiroides Hashimoto. Providers can offer guidance on treatment options, lifestyle modifications, and strategies for managing symptoms and improving quality of life.
Frequently Asked Questions
Here are some common questions and answers related to Tiroides Hashimoto:
What is the primary cause of Tiroides Hashimoto?
Tiroides Hashimoto is primarily caused by an autoimmune response where the immune system mistakenly attacks the thyroid gland, leading to inflammation and impaired hormone production.
Can Tiroides Hashimoto be cured?
While there is no cure for Tiroides Hashimoto, the condition can be effectively managed with thyroid hormone replacement therapy and lifestyle modifications.
Is Tiroides Hashimoto hereditary?
There is a genetic component to Tiroides Hashimoto, and individuals with a family history of the disorder or other autoimmune diseases may be at higher risk.
How is Tiroides Hashimoto diagnosed?
Diagnosis typically involves a combination of clinical evaluation, blood tests to measure thyroid hormone levels and antibodies, and sometimes imaging studies to assess the thyroid gland.
What are the common symptoms of Tiroides Hashimoto?
Common symptoms include fatigue, weight gain, cold intolerance, depression, and muscle weakness. Some individuals may also experience a goiter or swelling in the neck.
Are there dietary changes that can help manage Tiroides Hashimoto?
While no specific diet can cure Tiroides Hashimoto, a balanced diet rich in nutrients and low in goitrogens may support thyroid function and overall health.
Conclusion
Tiroides Hashimoto is a complex autoimmune disorder that affects millions of people worldwide. By understanding its causes, symptoms, and treatment options, individuals can take proactive steps to manage the condition and improve their quality of life. Ongoing research and advancements in medical care continue to offer hope for better management and outcomes for those living with Tiroides Hashimoto. With the right support and resources, patients can lead fulfilling lives and effectively navigate the challenges posed by this chronic condition.
Article Recommendations